Do You Know What An STI Looks Like?
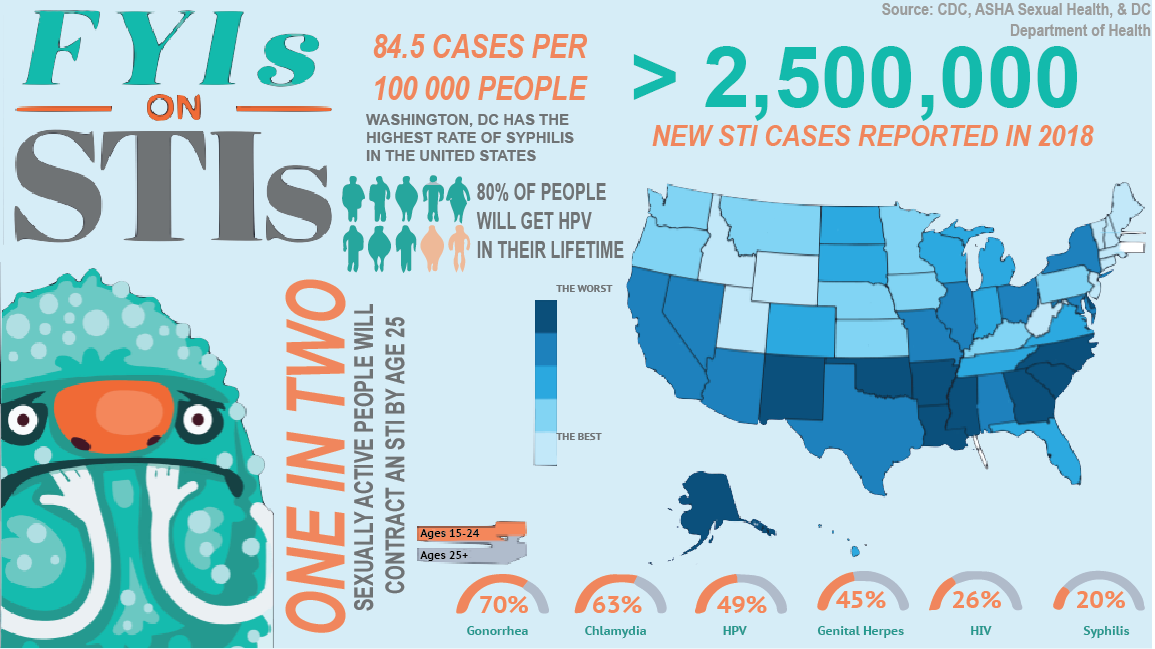
Sexually transmitted infections (STI) are extremely common, however, no one seems to want to acknowledge this. Because of this population silence, many people do not know what may be a common sign of an STI. Or worse, they choose to ignore it and hope it goes away on it’s own. Here are some signs and symptoms of the four most common STIs within Washington, DC and what kind of treatments are available for them.
STIs
Sexually transmitted infections (STI) are infections that are passed from one person to another during vaginal, anal, and oral sex. They are extremely common, and many people who have them end up not developing any symptoms. This makes some STIs more dangerous, but luckily there are easy tests that can be done and then treating them is even easier.


Do You Know the Risk?
Exposure to Blood or Menses
There is an EXTRA HIGH risk of contracting an STI when exposed to blood during any form of sexual intercourse.
Having direct exposure to someone else’s wounds, genital sores, or general abrasions while having sex is one of the highest risks one can put themselves at for developing an STI. STI’s are transmitted through bacteria and/or viruses traveling through the mucosal membrane– which is found throughout the genital tract– and into the blood stream.
Vaginal or Anal Sex
High Risk
Any time an individual has sex– no matter the form– they’re at risk for developing an STI. Because of the invasiveness that comes with anal sex, the risk for developing an STI is slightly higher than that of vaginal sex due to the risk of tearing being higher which would leave the mucosal membrane more susceptible to bacteria or viruses entering into the compromised blood vessel. Vaginal sex still has a high risk of developing an STI, however, due to the genital tract having a higher surface area.
Bare Frottage or Tribbing
Medium Risk
The risk of rubbing bare genitalia together varies based bodily fluids present. However, because semen and other bodily fluids have a possibility to be present and spread there is still a risk to be aware of. Depending on the STI, though, not all bacteria is able to survive outside of the body for even a moment, so the overall risk is slightly unknown.
Oral Sex
Medium Risk
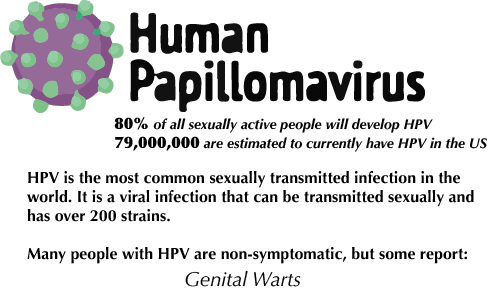
While not two genital regions are involved in this action, there are still STIs in which can develop outside of the genital region. Oral herpes, various strains of HPV, and even gonorrhea can be transmitted via the oral cavity. Similar to the genital tract, the oral cavity is surrounded by a mucosal membrane which can become compromised and then evaded by STI pathogens.
Hand Jobs or Fingering
Low Risk
Manual sex has an extremely low risk factor of developing an STI. This is because there is no direct contact of bodily fluids amongst all involved partners. It is important to note, though, that infections are still possible, however, more likely a UTI which is not classified as an STI.
Using Sex Toys
Low Risk
STI bacteria and viruses typically cannot survive outside of the body for long periods of time, so the ability for STI’s to be passed via this mechanism are extremely low. However, if the sex toys are not properly stored and kept sanitized, there is a high risk for developing a UTI.
Kissing
Low Risk
While saliva is considered a bodily fluid, it is filled with many protective barriers that make the passage of STIs extremely rare in almost all instances. The only STI capable of being passed via kissing is oral herpes, however, herpes is one of the most treatable STIs.
Do You Think You Need To Get Tested?
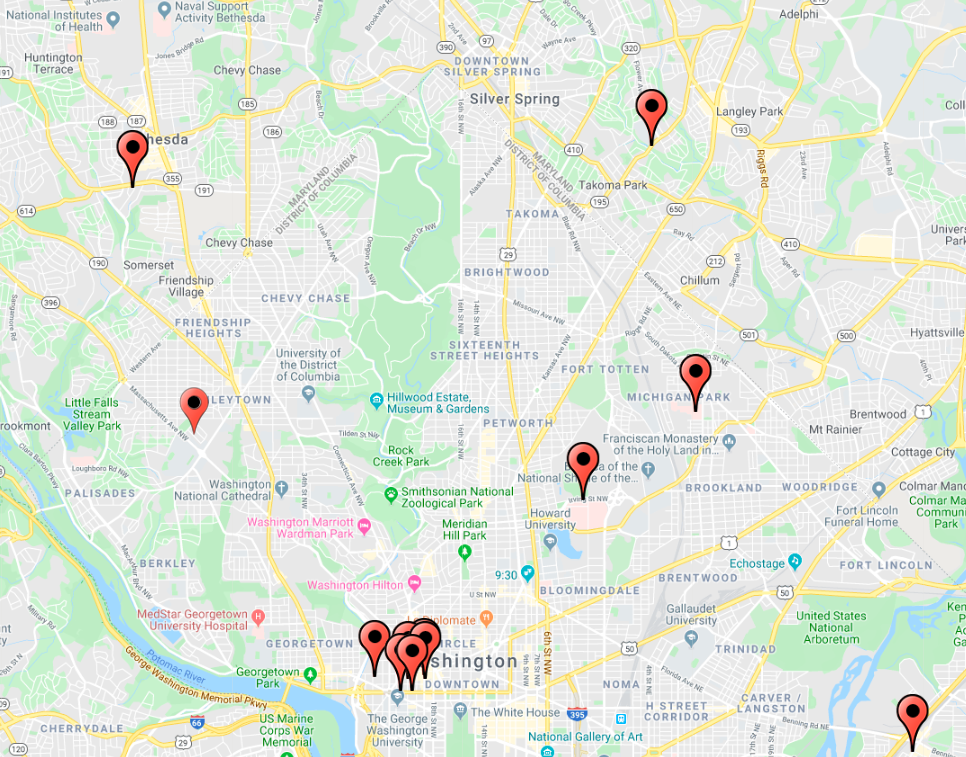
Where Can You Find A Testing Facility?
Frequently Asked Questions
What's the difference between STDs and STIs?
In short, there isn’t a difference. Sexually transmitted diseases (STDs) and sexually transmitted infections (STIs) are both entities which are transmitted through sexual interactions, however, in recent years there has been a shift from using the term “disease” because of the negative connotation it may hold.
How often should I be screened for STIs?
It is recommended by the CDC that all sexually active people should be screened for STIs at least once a year, but this is also dependent on the number of sexual partners one has or if they have more than one partner at a time.
More information can be found on the Center for Disease Control and Prevention website.
What can I do to protect myself from STIs?
The only way to completely protect yourself from STIs is to abstain from sex, however, there are other preventative measures that can highly reduce the risk of contracting an STI. External condoms when used properly have a 99% effectiveness rate. There are other internal condoms and dental dams which are highly efficient as well.
Can STIs be treated?
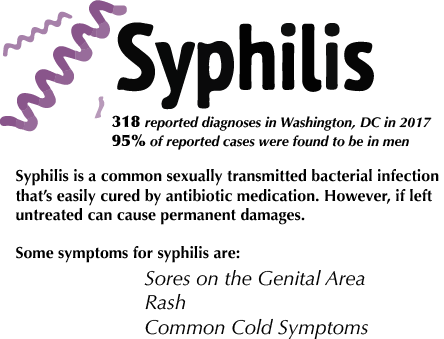
Almost all STIs can be treated, including syphilis, chlamydia, and gonorrhea which can all be cured. Other STIs such as herpes and HIV cannot be cured, but they can be highly managed due to new advancements in medicine.
Now That We Understand More About STIs, How Can We Prevent Them?
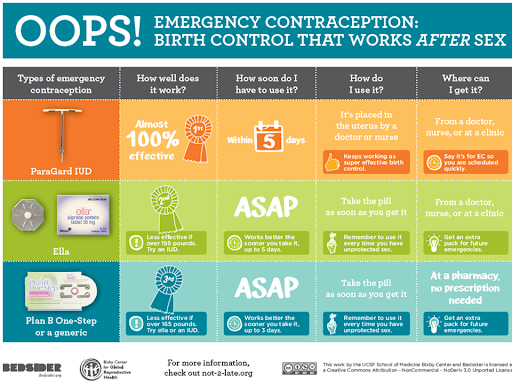
There are many contraceptive and barrier methods available for people looking to prevent pregnancy or sexually transmitted infections! Only one contraceptive method- other than abstinence- prevents both pregnancy and STIs (condoms), but there are many strategies for contraception which may be appropriate! If you are curious about a technique and whether it may be suitable for you, talk to your medical provider. Included below (courtesy of Bedsider.org) are the three emergency contraceptive methods available in the District of Columbia in instances of contraceptive failure, misuse, or non-use.
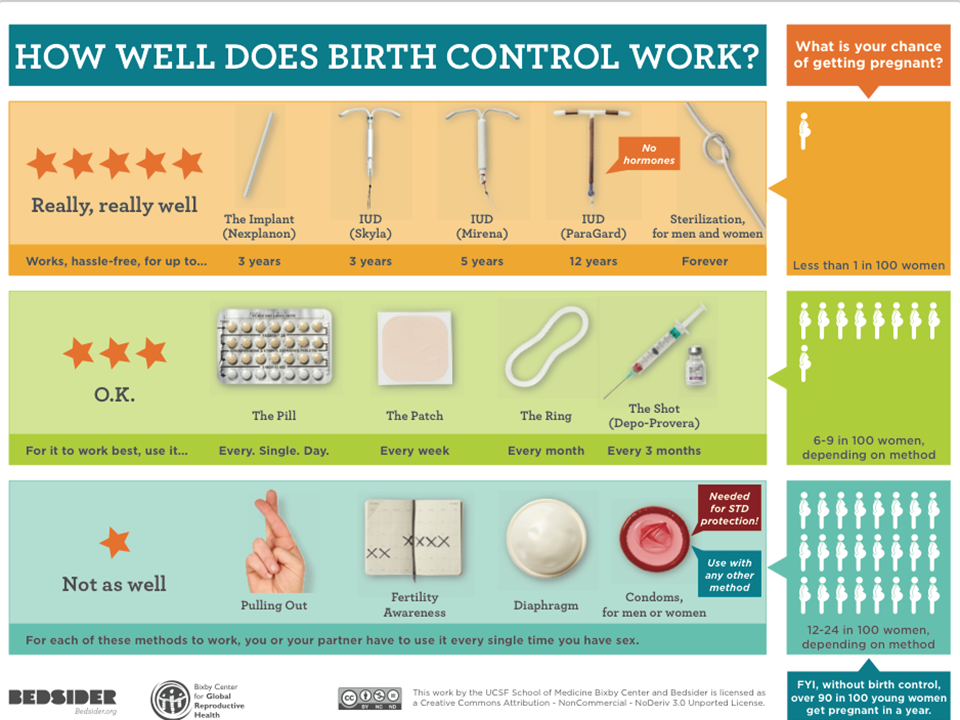
What Birth Control is Best for You?
Daily Oral Contraceptives ("The Pill")
Daily oral contraceptives exist in two varieties: combination pills and single-hormone (progestin) pills. Daily oral contraceptives require a prescription and the ability to stick to a strict schedule; this method is less effective when the pills are ingested at different times, or when days are missed. Oral contraceptives do not prevent against sexually transmitted infections.
Condoms
There are two kinds of condoms: external (commonly referred to as “male”) and internal (otherwise called “female”) condoms. Condoms are the only contraceptive method which prevent both pregnancy and sexually transmitted infections. There are many specialized condoms available for purchase (lubricated or not, ribbed or not, latex-free, flavored, etc.), but it is important to note that bearskin condoms do not block transmission of STIs.
Intrauterine Devices (IUDs)
IUDs are contraceptive devices implanted inside a uterus; they are a small, t-shaped piece of material which embeds in the wall of the uterus to prevent a fertilized egg from developing into a fetus. Several variations of IUDs exist, each working for either 3 to 12 years depending on selected model. If you think an IUD is the right fit for you and your partner, you should go see a gynecologist to speak about the procedure! IUDs do not prevent transmission of sexually transmitted infections.
The Patch & The Shot
The shot is a progestin injection which provides birth control for three months. It requires a prescription but, depending on provider and brand, can be injected at home. The shot does not prevent sexually transmitted infections from being passed between partners.
The patch is an external birth control strategy which needs to be replaced each week. It looks like a large, square bandaid and is user-friendly, but only has a 90% efficacy rate. The patch does not prevent transmission of STIs.
Want to Learn More About Birth Control Options?
Organizations such as Bedsider have built comprehensive and customizable online databases to explore efficacy rates, delivery strategies, and more!
References
Center for Disease Control and Prevention. (2017). Gonorrhea. Retrieved November 19, 2019 from: https://www.cdc.gov/std/gonorrhea/
Center for Disease Control and Prevention. (2018). Syphilis. Retrieved November 19, 2019 from: https://www.cdc.gov/std/syphilis/
Center for Disease Control and Prevention. (2019). HPV. Retrieved November 19, 2019 from: https://www.cdc.gov/hpv/index.html
Center for Disease Control and Prevention. (2017). Chlamydia. Retrieved November 19, 2019 from: https://www.cdc.gov/std/chlamydia/
DC Health. (2019).Annual Epidemiology & Surveillance Report: HAHSTA. Retrieved November 19, 2019 from: https://dchealth.dc.gov
Planned Parenthood. (2019). What Are STDs? Retrieved November 19, 2019 from: https://www.plannedparenthood.org/learn/
